Laparoscopy and laparoscopic surgery
 |
What is laparoscopy ?
Laparoscopy ( also called endoscopy or pelviscopy) is a surgical procedure in which a telescope is inserted inside the abdomen through a small cut below the navel, so that the doctor can have a look at the pelvic organs in the infertile woman. A laparoscopy can lead to the diagnosis of many problems which cause infertility including damaged tubes, endometriosis, adhesions and tuberculosis.
When is laparoscopy done?
In the past, a diagnostic laparoscopy was a routine part of the workup in infertile women, in order to complete their evaluation. Generally, the procedure was performed after the basic infertility tests were done, since it is a surgical ( invasive) procedure. Today, however, the utility of laparoscopy in treating infertile women is very limited, and we rarely perform laparoscopies in our clinic.
Timing the surgery
Some doctors will time the laparoscopy during the premenstrual phase (the week before the next period is due). They combine the laparoscopy with a dilatation and curettage (D & C) (scraping the inside of the uterine cavity) so that they can also get information on the woman’s ovulatory status in the same procedure.
Some doctors try to perform the diagnostic laparoscopy during the post-menstrual phase , when the uterine lining is thin, so that they can combine it with a hysteroscopy at the same time.
What precautions need to be taken before laparoscopic surgery ?
The patient is advised not to eat or drink anything for a specific time before the operation. Some tests may also be done before the procedure, to ensure safety for anesthesia, though for most young healthy women tests are usually not needed. Some doctors may want a HSG (hysterosalpingogram) done before performing a laparoscopy.
The surgery is usually done on a day-care basis. Laparoscopy is done under general anesthesia so that the patient remains asleep during surgery and does not feel any discomfort.
How is the laparoscopy performed ?
The laparoscopic procedure
First of all, the abdomen is cleansed and draped for the procedure. Then an instrument may be placed in the uterus through the vagina. A gas, such as carbon dioxide or nitrous oxide or air is then allowed to flow into the abdomen just below the belly button. This gas creates a space inside by pushing the abdominal wall and the bowel away from the organs in the pelvic area and makes it easier to see the reproductive organs clearly.
The laparoscope, which is a slender tube, like a miniature telescope, is then inserted through a small incision just below the navel. During the laparoscopy a small probe is placed through another incision in order to move the pelvic organs into clear view. A diagnostic laparoscopy is incomplete without a “second puncture” because, without this second probe, it is not possible to visualize all the structures completely.
During the laparoscopy the entire pelvis is carefully scanned and the organs inspected systematically – the uterus; the ovaries; and the lining of the abdomen, called the peritoneum. In addition to looking for diseases affecting these structures, the doctor also looks for adhesions (bands of scar tissue), endometriosis and tubercles. In case abnormalities are found, the doctor can either try to correct them (operative laparoscopy), or take out bits of tissue for histologic examination (biopsy) with a biopsy forceps. A blue dye (methylene blue) is then injected through the uterus and fallopian tubes to check whether the tubes are open. When the surgery is complete, the gas is removed and one or two stitches inserted to close the incisions. Since the incisions are so small, often stitches are not needed and they can be closed with Band-Aids.
The laparoscopy is the most important examination for finding the cause of infertility. For example, it is difficult to observe adhesions and the condition of an ovary with a hysterosalpingography or by other general methods of examination. But for those cases, more than 90% of the cause(s) of problems are found by using the laparoscopy, so the patient can receive an appropriate treatment. During the examination, treatment can be administered at the same time. For example, if an adhesion is observed, the adhesion can be lysis during the observation. The laparoscopy is also used for observing sperm transport in the tubes. On the patient’s examination day, artificial insemination is performed, and the laparoscopy can check whether the spemium reaches the uterine tube or not. In other ways, the salpingoscopy and the hysteroscopy are used at the same time for thoroughly researching and examining the cause of infertility.
As stated earlier, along with laparoscopy, some doctors carry out a dilatation and curettage (D & C) and send the endometrial curettings for histologic examination to rule out the possibility of hidden tuberculosis, and also to find out if ovulation is taking place. Others will do a diagnostic hysteroscopy at the same time, to ensure that the uterine cavity is normal.
Most doctors today use videolaparoscopy, in which a video camera is connected to the laparoscope, so that what the surgeon sees can be displayed on a TV monitor. This kind of laparoscopy can be very useful for documentation and record-keeping. It is also very helpful for patient education, since the doctors can use the video or CD later on to explain to the patient the exact nature of her problem.
Recent advances in miniaturization have allowed companies to manufacture very tiny laparoscopes. These are as thin as a needle, and are called microlaparoscopes or needlescopes. These allow doctors to perform laparoscopy in the clinic itself, without using anesthesia. However, the quality of the images is still not very good with these tiny scopes.
Dr Brosens from Belgium has also introduced the technique of transvaginal hydrolaparoscopy. This allows the doctor to examine the pelvis by inserting a tiny scope through the vagina, so that no abdominal incision needs to be made. The value of this technique as compared to conventional laparoscopy is still being studied.
What is an operative laparoscopy ?
During operative laparoscopy, many problems which cause infertility can be safely treated through the laparoscope at the same time that the diagnosis is made. When performing operative laparoscopy, additional instruments such as probes, scissors, biopsy forceps, coagulators and suture materials are placed into the abdomen, either through the laparoscope or through two or three additional incisions called “suprapubic punctures”, which are made above the pubis.
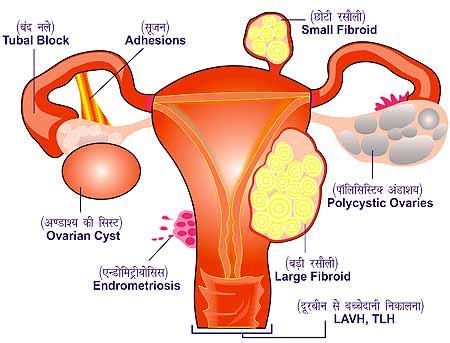
Some of the disorders that can be corrected with the help of the procedures above include: releasing scar tissue and/or adhesions from around the fallopian tubes and ovaries; opening blocked tubes; and removing ovarian cysts. Endometriosis can also be destroyed by burning it from the back of the uterus, ovaries, or peritoneum during operative laparoscopy. Under certain circumstances, small fibroid tumors can be removed and ectopic pregnancies can be treated.
When performing operative laparoscopy, surgeons may use electrocautery instruments, lasers, and sutures. The choice of the technique used depends on many factors including the surgeon’s training, location of the problem, and availability of equipment.
In this video, you can watch Dr Anjali Malpani perform an operative laparoscopy , in which she performs drills the ovaries to treat a patient with PCOD ( polycystic ovarian disease).
What is a “second-look laparoscopy ? “
Sometimes, a “second-look” laparoscopy may be recommended. This procedure is performed following either operative laparoscopy or major tubal surgery. Second-look laparoscopy can take place within a few days following the initial surgery or many months afterwards. During the procedure, the doctor determines whether adhesions are re-forming or if endometriosis is returning and these conditions can be treated in needed.
After surgery, the patient needs to rest for about 2 to 4 hours in order to recover from the effects of anesthesia. She can usually go home the same day and resume normal work in 2 to 3 days. Sexual activity can be resumed in a week or so, depending upon the doctor’s advice.
What can you expect to feel after the laparoscopy ?
After the operation, there may be some discomfort. This may include:
Mild nausea as a result of the medication or the surgical procedure
Pain in the neck and shoulder due to the gas inside the abdomen, which irritates the phrenic nerve and causes “referred pain” perceived in the shoulder
Pain in the areas where the instruments passed through the abdominal wall
A scratchy throat and hoarse voice if a breathing tube was used during general anesthesia
Cramps, like menstrual cramps
Discharge like a menstrual flow for a day or two
Muscle aches
Most of these minor symptoms will disappear within a day or two after surgery. The abdomen may feel swollen for a few days. Any unusual or peculiar symptoms should be reported at once to the doctor.
To really appreciate the benefits of laparoscopy, one should remember that the alternative is major surgery (laparotomy) which involves a large abdominal incision, a four to six day hospital stay, and four to six weeks of postoperative recovery time.
What are the complications of laparoscopy ?
While the doctors may term laparoscopy as being “minor” surgery, remember that for the patient all surgery is major! The risk of laparoscopy are minimal. But certain conditions increase the possibility of complications. If there has been previous surgery in the abdomen, especially involving the bowel, there is an increased risk. Other conditions that lead to a higher risk of complications are evidence of an infection in the abdomen, a large growth or tumor within the abdomen, and obesity.
Complications among young, healthy women under going laparoscopy are rare and occur only in about three out of 1000 cases. These complications can include injuries to structures in the abdomen such as the bowel, a blood vessel or the bladder. Most often, these injuries occur when the laparoscope is placed through the navel. If such an injury occurs during the procedure, the physician can perform major surgery and correct the damage through a longer abdominal incision. Sometimes, complications may arise after surgery. If bleeding or pain appears excessive or if high fever develops, the doctor should be informed.
How can I be sure my doctor will perform the laparoscopy properly ?
Unfortunately, many gynecologists are not skilled at performing a laparoscopy properly. In order to choose the best doctor for performing your laparoscopy, you need to ask him the following questions.
How many laparoscopies have you done?
Do you use multiple punctures?
Do you use a video for recording the operation?
If you find a problem, will you correct it at the same time? Ideally, if the doctor finds a problem during the laparoscopy, he should correct it at the same time, rather than call you again for a second surgical procedure, which only adds to your expense and risk.
A good doctor has a lot of experience in performing laparoscopies; uses multiple punctures, so he can assess the pelvis properly; and always provides documentation ( in the form of a video, CD or DVD) so the findings can be reviewed by another doctor.
Which is better – a laparoscopy or a HSG ?
Comparing laparoscopy and HSG
In our practise, we prefer using an HSG to document tubal patency, because it is much less expensive; is non-surgical; and provides a hard copy record , which all doctors can refer to later on. Some doctors still believe that both the HSG and laparoscopy are complementary procedures, and you may even need both, especially if your tubes are blocked. HSG provides information only about the inside of the tubes and uterine cavity, whereas in laparoscopy, not only can the tubal patency be determined, but two other disorders ( endometriosis and tubal adhesions) inside the abdomen which affect tubal function and which do not show up on HSG can also be diagnosed. However, while it is true that a laparoscopy offers the doctor a chance to diagnose and treat these problems at the same time , it is still unsure whether correcting these problems actually helps to improve the patient’s fertility !
A common problem which patients face in practice is that many doctors will insist on repeating the laparoscopy. One reason for this is that doctors feel that they need to do the laparoscopy for themselves, because they cannot “trust” another doctor’s judgment. This is, of course a major problem for patients, who suffer repeated (and unnecessary) laparoscopies. Having a video record should help to minimize this problem.
What happens if your laparoscopy was normal and the second doctor wants to repeat it anyway? Sometimes doctors have little to offer in the way of effective treatment and since there is nothing else to do, they suggest a repeat laparoscopy to which the hapless patient is forced to agree. If your first laparoscopy did, in fact indicate you had a problem, a second look laparoscopy may be indicated (and this should have been discussed with you after the first laparoscopy) to determine if the problem has been successfully resolved. Ask the doctor what information he hopes to get by doing the repeat laparoscopy and how this will change your treatment. If you feel the doctor wants to do a laparoscopy for no very good reason, refuse. It’s a surgical procedure after all – and it’s your body.
Thinking it over
One benefit of laparoscopy is that in addition to allowing the accurate diagnosis of a problem, if it exists, operative laparoscopy can also be done in the same surgery to correct the problem. However, we feel that the routine use of laparoscopy is not called for in treating infertile patients, since a HSG can provide similar information at much less risk and expense. We use the procedure very sparingly in our practise.
 |
Hysteroscopy
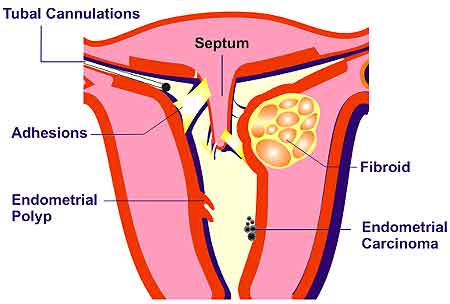
Hysteroscopy, as the name suggests (hystero = uterus; scopy = to see), is a surgical procedure in which a telescope is inserted inside the uterus to examine the uterine lining. This procedure can assist in the diagnosis of various uterine conditions which can cause infertility, such as:
1.submucous (internal) fibroids
2.scarring (adhesions or synechiae)
3.endometrial polyps
4.uterine septa and other congenital malformations
Before performing hysteroscopy, a hysterosalpingogram (an x-ray of the uterus and fallopian tubes) may be performed to provide additional information about the cavity which can be useful during surgery. Many doctors will also do a vaginal ultrasound as a diagnostic aid. Diagnostic hysteroscopy is usually conducted on a day-care basis with either general or local anesthesia and takes about thirty minutes to perform.
How is hysteroscopy performed ?
The first step of hysteroscopy involves cervical dilatation – stretching and opening the canal of the cervix with a series of dilators. Once the dilatation of the cervix is complete, the hysteroscope, a narrow lighted telescope, is passed through the cervix and into the lower end of the uterus. A clear solution (Hyskon or glycine) or carbon dioxide gas is then injected into the uterus through the instrument. This solution or gas expands the uterine cavity, clears blood and mucus away, and enables the surgeon to directly view the internal structure of the uterus.
The doctor systematically examines the lining of the cervical canal; the lining of the uterine cavity; and looks for the internal openings of the fallopian tubes where they enter the uterine cavity – the tubal ostia.
Some doctors may do a curettage (a surgical scraping of the inside of the uterine cavity) after the hysteroscopy and send the endometrial tissue for pathologic examination.
What is operative hysteroscopy ?
The technique of hysteroscopy has also been expanded to include operative hysteroscopy. Operative hysteroscopy can treat many of the abnormalities found during diagnostic hysteroscopy at the time of diagnosis.
The procedure is very similar to diagnostic hysteroscopy except that operating instruments such as scissors, biopsy forceps, electocautery instruments, and graspers can be placed into the uterine cavity through a channel in the operative hysteroscope. Fibroid tumors, scar tissue (synechiae or adhesions), and polyps can be removed from inside the uterus. Congenital abnormalities, such as a uterine septum, may also be corrected through the hysteroscope.
In this video, you can watch Dr Anjali Malpani perform an operative hysteroscopy, in which she performs an adhesiolysis to remove intrauterine adhesions to treat Asherman syndrome
What is hysteroscopic tubal cannulation ?
A relatively new method for treating proximal tubal obstruction (cornual blocks, where the tubes are blocked at the utero-tubal junction) is that of hysteroscopic tubal cannulation. Many studies have shown that this kind of block is often because of mucus plugs or debris which plug the tubal lining at the uterotubal junction which is as thin as a hair. It is now possible to pass a fine guidewire through the hysteroscope into the tubes, and thus remove the plug or debris and open the tubes – thus restoring normal tubal patency with “minimally invasive surgery”!
Another advance has been the development of the method of falloposcopy – in which a very fine flexible telescope is passed into the tube through the hysteroscope, so as to visualize the interior of the entire tube.
After a hysteroscopy, patients often have cramping similar to that experienced during a menstrual period; and some vaginal staining for several days. Regular activities can be resumed within one or two days after surgery. Sexual intercourse should be avoided for a few days or for as long as bleeding occurs.
What are the complications of hysteroscopy ?
Complications occur rarely during hysteroscopy. In a few cases, infection of the uterus or fallopian tubes can result. Occasionally, a hole may be made through the back of the uterus – a perforation. However, this is usually not a serious problem because the perforation closes on its own. Frequently, when extensive operative hysteroscopy is planned, diagnostic laparoscopy is performed at the same time to allow the surgeon to see the outside as well as the inside of the uterus to try to reduce the risk of accidental uterine perforation. Other possible complications include allergic reactions and bleeding.
What are uterine( endometrial) polyps ?
Polyps
Endometrial or uterine polyps are soft, fingerlike growths which develop in the lining of the uterus (the endometrium). They develop because of excessive multiplication of the endometrial cells, and are hormonally dependent , so that they increase in size depending upon the estrogen level. They can usually be detected on an ultrasound scan if this is done mid-cycle, when estrogen levels are maximal, but are easily missed if the scan is not done at the right time of the menstrual cycle. Polyps are an uncommon but important cause of infertility, because they can easily be removed during hysteroscopic surgery.
How do fibroids ( myomas) affect fertility ?
Fibroids
While the commonest problem found in the uterus is a fibroid (myoma or leiomyoma), this is rarely a cause of infertility, and is usually an incidental finding of little importance. Fibroids are common benign smooth muscle tumors which arise in the wall of the uterus, and may be single or multiple. About 25% of all women over the age of 35 have fibroids.
Most fibroids develop in the wall of the uterus (intramural ) or protrude outside of the uterine wall (subserous fibroids), and these can usually be left alone, since they do not hinder fertility, and neither do they cause problems during the pregnancy. In fact, unnecessary surgery to remove the fibroid often causes more harm than good. This surgery often creates adhesions, which causes the tubes to get blocked.
However, if the fibroids are very large, they may need surgical removal, and this procedure is called a myomectomy. Some doctors give an injection of a GnRH analog prior to surgery in order to shrink the fibroid and make surgery technically easier. When performed by an expert, it is a safe and effective procedure which can be accomplished with minimal blood loss. However, sometimes because of uncontrollable bleeding the surgeon may be forced to remove the entire uterus (a procedure called a hysterectomy), and this is obviously a disaster for the infertile woman!
The standard technique for removing a fibroid is through open surgery (laparotomy). It is now also possible to remove fibroids through the laparoscope, but laparoscopic myomectomy does not allow for optimal reconstruction of the uterus. Submucous fibroids are an important cause of infertility, because they interfere with implantation of the embryo, by acting as a foreign body. These are best removed by an operative hysteroscopy. While surgery can remove the fibroid, it can recur again, and most doctors advise the patient to try to conceive as soon as possible after surgery
Fibroids may grow larger during the pregnancy, but usually pregnancy and delivery are uneventful. In rare cases, after a myomectomy, uterine rupture may occur during pregnancy or delivery, and this complication may result in severe blood loss, fetal loss and even maternal death.
Because of the potential for catastrophic results, it is recommended that women have cesarean deliveries in the following circumstances: 1) when the myomectomy involved full-thickness incision of the uterine wall or multiple deep uterine incisions or 2) when myomectomy was complicated by infection which may have weakened the uterine wall or 3) when there is doubt regarding the adequacy or extent of the uterine repair.
The uterus was often a neglected organ in the infertility workup, partly because we did not have the tools to study it properly. Hysteroscopy, hysterosalpingography and vaginal ultrasound are all complementary procedures for evaluating the uterine cavity in the infertile woman. The HSG is good for looking for polyps, adhesions and septa which appear as “filling defects” on the X-ray. However, careful radiologic technique is a must. Vaginal ultrasound is excellent for detecting submucosal fibroids or polyps, which can be missed on hysteroscopy and HSG. Of course, the major advantage of hysteroscopy is it offers the chance of treating the problem as well!
What are the new techniques for studying the role of the endometrium in infertility ?
We are now also developing newer techniques to study the uterus. One of our major areas of ignorance today is the complex process of embryo implantation. It is obvious that the endometrium has a key role to play in this process, in which the embryo has to appose and attach itself to the maternal endometrium and invade into it. At present, the tools we have to study endometrial function and receptivity are very crude. They include primarily transvaginal ultrasound, to assess the endometrial thickness and texture, but this provides very limited and indirect evidence of endometrial functions. Colour Doppler ultrasound has also been used to assess endometrial blood flow ( perfusion), but its utility is limited.
Since embryo-endometrium interaction is a biochemical process, a lot of study has been done on the role of the molecules involved in this process. Recent research has shown that the normal endometrium contains various cell adhesion proteins called integrins, which allow the embryo to interact with it. Studies have shown that the endometrium of some infertile women is deficient in some of these integrins, and this deficiency may be responsible for failure of the embryo to implant successfully. Thus, testing the endometrium for beta integrin can be a useful marker for uterine receptivity. This test involves doing an endometrial biopsy at a specific point in the menstrual cycle, and evaluating this with special staining techniques, but is only available on a research basis so far.

