|
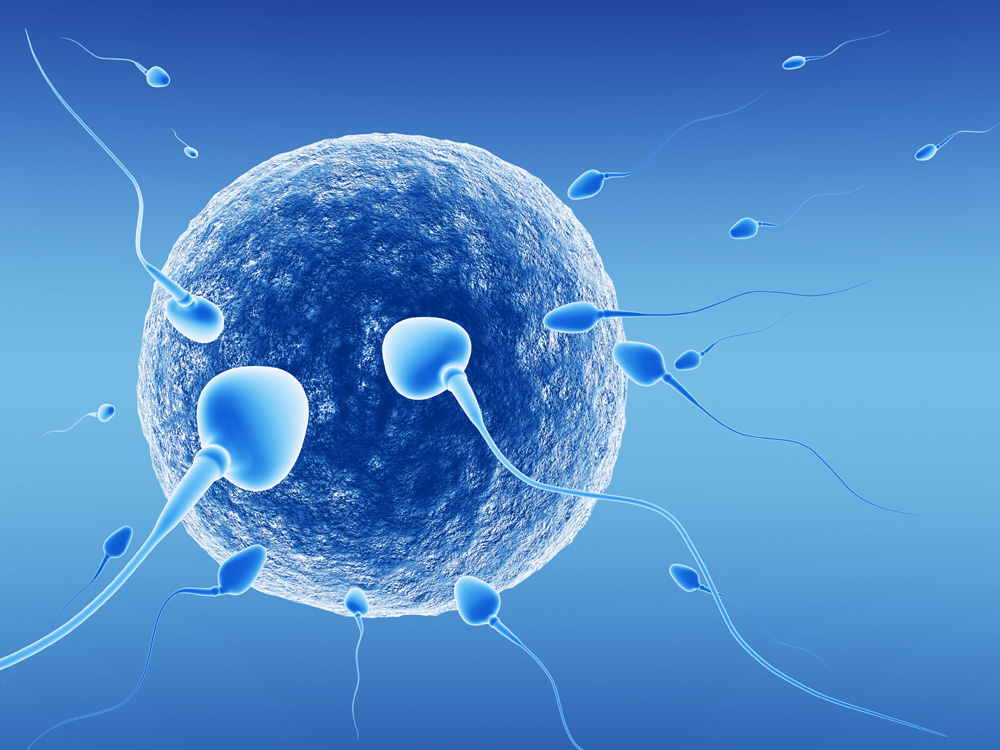
In Vitro Fertilization (IVF) has become the cornerstone of reproductive medicine, and IVF clinics today routinely perform techniques which were thought to belong to the realm of science fiction a generation ago! IVF is the basic assisted reproduction technique, in which fertilization occurs in vitro (literally, in glass). The man’s sperm and the woman’s egg are combined in a laboratory dish, and after fertilization, the resulting embryo is then transferred to the woman’s uterus. The five basic steps in an IVF treatment cycle are superovulation (stimulating the development of more than one egg in a cycle), egg retrieval, fertilization, embryo culture, IVF is a treatment option for couples with various types of infertility, since it allows the doctor to perform in the laboratory what is not happening in the bedroom – we no longer have to leave everything upto chance! Initially, IVF was only used when the woman had blocked, damaged, or absent fallopian tubes (tubal factor infertility). Today, IVF is used to circumvent infertility caused by practically any problem, including endometriosis; immunological problems; unexplained infertility; and male factor infertility. It is a final common pathway, since it allows the doctor to bypass nature’s hurdles and overcome its inefficiency, so that we can give Nature a helping hand! In order to perform IVF, only 3 things are required – eggs, sperm and a uterus, and before starting the IVF cycle, the doctor will check these. First, a sperm survival test is carried out This is a “trial” sperm wash, using exactly the same method as will be actually used in IVF, to assess whether an adequate number of sperm can be recovered in order to do IVF. This test will also help the laboratory to decide which method of sperm processing should be used during IVF. A blood FSH level will provide an idea of the “ovarian reserve”, and provide information on whether or not the woman will produce enough eggs after Many clinics may do a hysteroscopy, in order to assess that the uterine cavity is totally normal. They may also do a “dummy” embryo transfer to make sure there are no technical problems with this procedure. Some clinics also do a cervical swab test, to rule out the presence of infection in the cervix. If a woman has blocked fallopian tubes with large hydrosalpinges, some clinics will remove these prior to the IVF cycle, because they feel that the presence of a hydrosalpinx decreases pregnancy rates after IVF. For men who have difficulty in producing a semen sample “on demand”, the clinic may also freeze and store the sample prior to treatment, as a backup. This can help to prevent the tragedy of having to abort an entire treatment cycle because the man could not produce a semen sample when needed. Blood tests which may be done include tests for immunity to rubella; and tests for Hepatitis B, and AIDS. Most doctors will also advise patients to start taking folic acid, as part of pre-pregnancy care, as this helps to reduce the risk of certain birth defects. Patients who stand a very poor chance of success with IVF include the following:
|